Thyroid eye disease (TED) is a complex disease that can lead to significant ocular symptoms, facial disfigurement, and decreased quality of life. Most patients with TED have hyperthyroidism with the most common cause being Graves’ disease. TED may also occur in patients with hypothyroidism (Hashimoto’s thyroiditis) or euthyroidism. It affects 16 per 100,000 females and 2.9 per 100,000 males. Female gender, middle age, and smoking all have been associated with increased risk for TED.
TED is characterized by changes in the orbital soft tissue, including inflammation and remodeling. A subset of CD34+ fibrocytes infiltrate the orbit and express high levels of thyroid-stimulating hormone receptors (TSHR). These cells can differentiate into either fat cells or myofibroblasts which results in the two subtypes of TED: fat-predominant or muscle-predominant disease respectively.
The disease shows an acute inflammatory or active phase, to begin with, lasting on average for about 18 months. The inflammation then gradually subsides and the patient enters a more chronic or stable phase characterized by fibrosis.
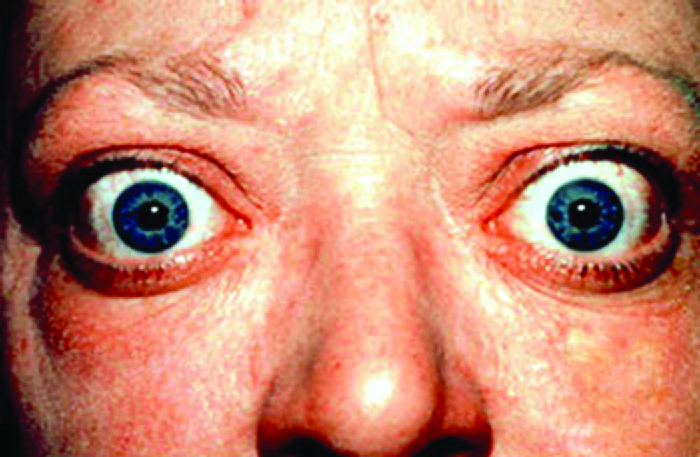
More than 90% of patients present with eyelid retraction, the most common clinical sign. Other signs include proptosis, lid lag of the upper eyelid on down gaze (von Graefe sign), eyelid edema and erythema, conjunctival congestion, chemosis, and restrictive strabismus. The clinical presentation may commonly include symptoms of dry eye disease. In severe disease, exposure keratopathy or compressive optic neuropathy may be present. The diagnosis of TED is based on the classical clinical picture and systemic thyroid dysfunction. Orbital imaging can be used to aid in the diagnosis of TED and classification into its subtypes. Orbital computed tomography (CT) scan or magnetic resonance imaging (MRI) may show extraocular muscle involvement. Classically, the muscle belly is enlarged but the tendon is spared. The inferior rectus muscle is most commonly involved.
TED is graded by the activity and severity of the disease. Activity refers to soft tissue changes and inflammatory symptoms. It is often assessed by the clinical activity score (CAS). Treatment depends on the patient’s disease activity and requires a multidisciplinary approach. Generally, treatment includes controlling thyroid hormone levels, lubricants, selenium supplementation, and minimizing risk factors that can exacerbate the disease such as smoking. Systemic corticosteroids are used in the treatment of active TED. Intravenous corticosteroids are more effective and better tolerated than oral corticosteroids. Other treatment options include systemic immunosuppressants and newer targeted therapies such as teprotumumab. Later, after the disease enters a stable phase, treatment often includes surgical correction of the residual proptosis, strabismus, and eyelid deformities.
In recent years, there have been exciting developments in the understanding and management of TED. Hence, we can expect a paradigm shift to more targeted and effective therapies in the near future.
Lazarus JH. Epidemiology of Graves’ orbitopathy (GO) and relationship with thyroid disease. Best Practice & Research Clinical Endocrinology & Metabolism. 2012;26:273-9.
Dosiou C, Kossler AL. Thyroid Eye Disease: Navigating the New Treatment Landscape. Journal of the Endocrine Society. 2021 May;5:5.
Picture courtesy: License: Creative Commons Attribution License (by 4.0) Authors: OpenStax Microbiology Copyright Holders: OpenStax Microbiology Publishers: OpenStax Microbiology Latest Version: 4.4